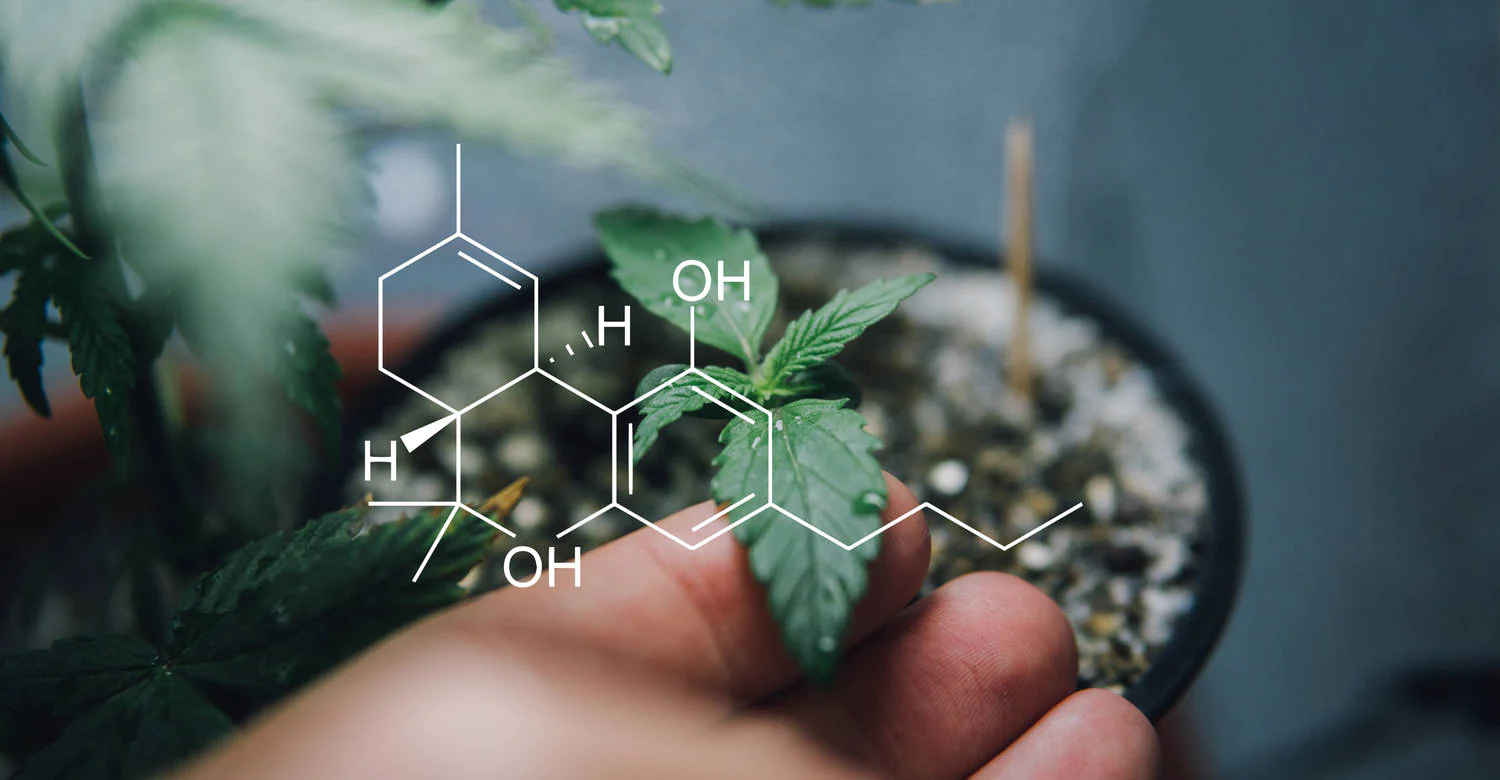
For thousands of years, people around the world have used cannabis for its many therapeutic and relaxing effects on our bodies. But only in the last century have we begun to gain a real understanding of exactly how this diverse plant can trigger these reactions. The discovery of the endocannabinoid system in the 20th century led to increased research not only into cannabis and its most common compounds - cannabinoids - but also into the many compounds produced within the body itself. This research has led to several important insights into the role of the endocannabinoid system and what this might mean for the development of new medical therapies.
The endocannabinoid system was first recognized after the discovery of two receptors in the body, now known as cannabinoid receptor 1 (CB1) and cannabinoid receptor 2 (CB2). To date, the ECS, including these two receptors, is involved in a number of vital cognitive and physiological functions in the human body.
What is the endocannabinoid system?
The endocannabinoid system consists of three main components: receptors (CB1 and CB2), enzymes and neurotransmitters that interact with the receptors. These neurotransmitters are produced naturally in our bodies and have a similar chemical structure to the cannabinoids produced by the cannabis plant - hence their name endocannabinoids.
Studies have shown how interactions between CB1 and CB2 receptors and endocannabinoids - as well as cannabinoids from the cannabis plant (phytocannabinoids) - can trigger a variety of responses that can affect mood, temperature regulation, pain signalling, fertility and much more.
The endocannabinoid system is distributed throughout the body, with CB1 and CB2 receptors found in the immune system, central nervous system and virtually every organ. The existence of specific cannabinoid receptors in the bodies of humans and animals had been debated for decades, but in the mid-1980s, scientists at St. Louis University claimed to have made some important findings that provided irrefutable evidence for the existence of such receptors.
This was confirmed in 1990 by cloning rat CB1 receptor 2 by Gérard and colleagues in Brussels and in 1993 by cloning CB2 in Sean Munro's lab in Cambridge. Since their discovery, we have learned a great deal about these receptors and the role they play in various bodily functions. Key findings include that CB1 receptors inhibit the release of transporters (endocannabinoids) in the body, while CB2 receptors likely modulate cytokine release and immune cell migration.
Neurotransmitters and the endocannabinoid system
Since the discovery of cannabinoid receptors, a number of endogenous cannabinoids have also been discovered, many of which can directly stimulate these receptors. In addition, phytocannabinoids such as THC, CBD and many others have also been found to interact with these receptors and potentially trigger a number of processes.
The development of synthetic cannabinoids has also been a growing area of cannabis research in recent decades. These laboratory-made compounds in turn have a similar chemical structure to endocannabinoids, allowing them to interact with cannabinoid receptors in our bodies.

Endocannabinoids: the body's natural cannabinoids
The neurotransmitters that naturally stimulate the CB1 and CB2 receptors in the human body are called endogenous cannabinoids - or endocannabinoids. The first of these endocannabinoids to be discovered was anandamide, named after the Sanskrit word ananda, meaning 'bliss'.
Anandamide (AEA) was discovered in 1992 and classified as a cannabinoid receptor agonist - but it was soon discovered that it was not the only endocannabinoid. In fact, scientists soon realized that mammalian tissue contains a number of other fatty acid derivatives that behave as endocannabinoids - the most studied of which is 2-arachidonoylglycerol (2-AG). There is evidence that these endocannabinoids are synthesized on demand rather than stored - most likely due to stimulation of cannabinoid receptors.
Now that we know the key components of the endocannabinoid system, let's take a closer look at how they work together. As mentioned, cannabinoid receptors (CB1 and CB2) are found throughout our bodies, including on the surface of immune cells and neurons. CB1 receptors are actually more numerous than many other types of receptors found in the brain. They essentially act as modulators, controlling the levels and activity of many other neurotransmitters - including, but not limited to, endocannabinoids.
Endocannabinoids, produced by our bodies to stimulate CB1 and CB2 receptors, are now thought to be crucial for controlling various functions. These compounds bind to cannabinoid receptor sites.
Function and regulation of the endocannabinoid system (ECS)
CB1 receptors are located primarily in the central nervous system. They have been found to regulate neuronal transmission and other important physiological processes, including pain, inflammation, memory and eating behaviour. This receptor can be activated by a variety of endogenous, synthetic and plant compounds, including endocannabinoids and THC.
In contrast, CB2 receptors are located primarily in the immune system, which may highlight a potential immunomodulatory role for the endocannabinoid system. Various in vitro and animal studies have shown that the CB2 receptor can modulate immune cell function in models of inflammatory diseases. Therefore, it is suggested that therapeutic approaches to modulate CB2 signaling may offer promising treatment options for inflammatory diseases such as rheumatoid arthritis and inflammatory bowel disease.
Much more research needs to be done to fully understand the exact physiological and neural mechanisms of the endocannabinoid system. However, it is now widely accepted that this receptor system plays a critical role in many important body functions, including memory and learning, sleep, temperature regulation, pain signaling, inflammatory and immune responses, and emotional processing. Dysregulation of the endocannabinoid system is also associated with a number of diseases, including obesity and neurodegenerative diseases, as well as schizophrenia.
There is evidence that exposure to cannabinoids is not the only thing that can regulate ECS activity. For example, exercise has been found to have a number of significant benefits for our health - including activating the release of endocannabinoids. A number of studies have shown that our bodies release endocannabinoids in response to high-intensity activities such as running. This increase in endocannabinoids has been reported to have an antinociceptive effect for a short period of time after exercise. This response, along with the effects of other neurotransmitters, is often referred to as "runner's high".
Other factors that have been shown to regulate ECS activity include stress and even dietary habits.
The discovery of the endocannabinoid system has led to accelerated research into the therapeutic and medicinal potential of phytocannabinoids such as CBD and THC. In recent decades, research on medicinal cannabis has experienced a tremendous boom after a period of stagnation during the long period of prohibition in the 20th century.
Much of this research has been driven by the need for alternative effective therapies for various diseases, including chronic pain, epilepsy and cancer. Existing treatments for these and many other diseases are often of questionable efficacy and carry significant risks of adverse side effects (e.g. the use of opioids for chronic pain). Further research into the potential role of endocannabinoids in such diseases is therefore an important area of research for the development of new treatments.
Medicinal cannabis is a widely recognised term that refers to medicinal products derived from the Cannabis Sativa plant. These can include cannabinoid extracts and even whole flower products. Cannabis has been used as a medicine to treat various ailments for thousands of years. However, it is only since the discovery of the endocannabinoid system that we have a better understanding of the mechanisms of action of medicinal cannabis - although there is still much to learn.
However, current evidence suggests that medicinal cannabis may be useful in the treatment of a number of diseases. In recent years, an increasing number of countries and jurisdictions have legalised medical cannabis so that it can be used to treat a variety of conditions such as chronic pain, multiple sclerosis, epilepsy and anxiety.
Chronic pain is the most frequently cited reason for the use of medicinal cannabis worldwide. Real-world data show that patients with chronic pain conditions often find medical cannabis to be a useful treatment for pain and associated symptoms of their disease, including anxiety and depression, and also for improving their quality of life. However, there is still a lack of good clinical evidence in this area.
In recent years, medical cannabis has increasingly been considered as a potential therapy for treatment-resistant epilepsy. A number of studies have demonstrated the anticonvulsant potential of medical cannabis, and in particular the non-toxic cannabinoid CBD. Medical cannabis (most commonly the CBD-based drug Epidyolex) is now approved in a number of countries around the world for the treatment of various forms of epilepsy.
There is also growing evidence that cannabis and its derivatives may be useful in treating a variety of other medical conditions. Encouraged by these studies, more and more consumers are turning to over-the-counter CBD products to treat a variety of ailments, including anxiety, stress, sleep problems, and overall well-being; however, it is important to note that there is a wide variation in quality among over-the-counter CBD products.
Given the perceived importance of the endocannabinoid system and the resulting role of endocannabinoids such as anandamide and 2-AG, many have theorized that a deficiency of these compounds could have significant effects on overall health. While evidence to support this theory has been lacking in the past, a 2016 study found reduced endocannabinoid levels and ECS hypofunction in a number of conditions, including migraines and post-traumatic stress disorder.
Although more research is needed to fully understand this phenomenon, some symptoms that could indicate endocannabinoid deficiency include lower pain thresholds and changes in mood and sleep(8).
There is no doubt that the endocannabinoid system plays an important role in our overall health and well-being. This receptor system is responsible for a number of key processes and functions that could make it a priority target in the development of future medical therapies and treatments.
